S1E3: Flatten the Curve / Craig Spencer & Helen Branswell
“The goal is to try to keep as many people from being infected for as long as possible to try to effectively stretch this thing out so that the hospitals are dealing with fewer cases.” – Helen Branswell
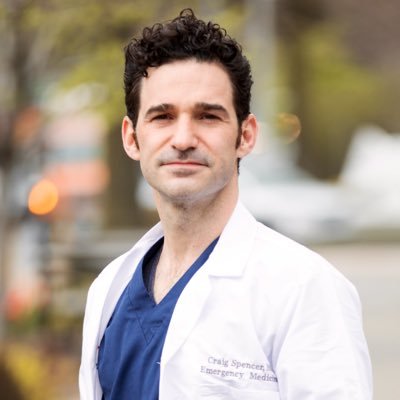
In today’s episode, co-hosts Dr. Celine Gounder and Ron Klain discuss the concept of flattening the curve and what impact this can have on healthcare workers and hospitals. They speak with Helen Branswell, a leading infectious disease reporter at STAT. Helen speaks about what other countries are doing to fight against the pandemic and flatten their own curves, and how these measures compare to measures currently being taken in the United States. The co-hosts also speak with Dr. Craig Spencer from Columbia University Medical Center, a member of the Board of Directors of Doctors Without Borders for the United States. Dr. Craig Spencer discusses his own experiences in working as a healthcare worker during other infectious disease outbreaks, including the Ebola epidemic in Guinea, where he himself became infected, but was successfully treated back home in the United States. He also talks about the kinds of tough choices that healthcare workers in the United States will soon have to face.
Listener Q&A: Should my 89-year old mother come to live with me in order to decrease her chances of becoming infected with COVID-19, or is it safer for her to isolate herself in her apartment? Why don’t state health departments take public health guidance on COVID-19 from WHO or academia, rather than the CDC and federal government? Would there be legal repercussions if states were to follow the recommendations of their own experts? Is there any evidence that moving college courses online will really slow the spread of the virus?
This podcast was created by Just Human Productions. We’re powered and distributed by Simplecast. We’re supported, in part, by listeners like you.
Celine Gounder: I’m Dr. Celine Gounder.
Ron Klain: And I’m Ron Klain
Celine Gounder: And this is “Epidemic.”
Ron Klain: Today is Friday, March 13th. In this episode, we’re going to talk about what we’re doing now and what we need to be doing to control the coronavirus pandemic.
Celine Gounder: You may have heard this expression flattening the curve. Well, when we talk about flattening the curve, what we really mean is we want to slow transmission of the coronavirus.100 patients in an emergency room in an hour is a very different scenario than a hundred patients in a day or a week.
Ron Klain: We’re going to talk in this episode about how healthcare workers are impacted by an epidemic like this, and we’re going to hear it from someone who knows. Dr. Craig Spencer works with Doctors Without Borders around the world. He’s been on the front lines of some of the worst epidemics and health crises around the world, and what’s more, he’s been a patient himself. While fighting Ebola in West Africa, he got Ebola and had to be brought back to the U.S. for treatment.
Celine Gounder: And finally, we’ll close with a few listener questions as we do every week. So today on the epidemic podcast, we’re delighted to welcome the leading infectious disease reporter in the world. Someone I read regularly, Helen Branswell of STAT. She’s the go-to source on the coronavirus pandemic. Helen, thanks for joining us on the podcast.
Helen Branswell: Thank you for inviting me.
Celine Gounder: Helen, I know you’ve been tracking some of the discussions at the World Health Organization and on Wednesday, Dr. Tedros Ghebreyesus, the Director General of WHO said, “we cannot say this loudly or clearly enough or often enough. All countries can still change the course of this pandemic.”
What is it that he was referring to? What is it that we can be doing?
Helen Branswell: What the WHO has been saying for weeks now, is that some countries have been able to effectively beat this thing back. I mean, if you look at what’s happening in China on, uh, March 11th, they recorded 15 cases, which is probably the lowest daily increase since, I don’t know, the second or third week of January.
So clearly, they’ve taken very, very draconian measures that many other countries would not feel they were able to do, but they have been able to be it back. So, what the WHO has been saying is this is not as uncontrollable as flu. This can be controlled if you really work very hard at it. That remains to be seen though in countries that don’t have the kinds of governments or social cohesion perhaps, that you might expect in places like China and South Korea.
Ron Klain: Dr. Mike Ryan, who leads the WHO emergency program here, you and I both know him, said on Wednesday that some countries are not doing enough, not responding adequately. And he said, quote, “you know who you are.” So, do we think Dr. Ryan was talking about the United States?
Helen Branswell: You know, I haven’t had a chance to talk to Mike, so I’m not certain who he was referring to. Uh, I doubt that it’s one country. There’s a great deal of frustration there that some countries seem to feel that trying to contain the virus is unworkable and that they should move to mitigation. And I think the WHO folks think that’s a disaster in the making and are really trying to exhort countries to, to work harder at trying to find cases and isolate, uh, them and quarantine their contacts and really work at this with those old fashioned public health tools.
Celine Gounder: So Helen, I have a question for you about that. Do we just tell people, if you have a fever and cough, you just stay home. Don’t even bother getting tested. We’re not even going to try to do contact tracing. You know? Are we at that point or should we be still doing some of these things Like WHO is advocating?
Helen Branswell: I would say that I find it interesting that, you know, in countries where they didn’t start off with the aggressive measures that China or South Korea or Japan or Singapore have been using, they’ve moved to them afterwards. Italy didn’t take that approach and found that it was so overwhelmed that it had to lockdown first the North, and now effectively the entire country.
Either you attack it aggressively early or you’re going to have to take really draconian measures afterwards seems to be what the pattern is.
Ron Klain: So Helen, this week, Tony Fauci testified before Congress, and I thought his tone and some of the things he said were about as anxious as I’ve seen in a very, very long time. This is what he said.
The stated mortality overall of this, when you look at all the data, including China, is about 3%. It first started off as two and now three. I think if you count all the cases of minimally symptomatic or asymptomatic infection, that probably brings the mortality rate down to somewhere around 1%, which means it is 10 times more lethal than the seasonal flu. I think that’s something that people can get their arms around and understand.
Ron Klain: What do you read in his remarks and what do you read about his level of concern about how seriously we’re taking this in the U.S.?
Helen Branswell: What do I make of it? I think it’s frankly time that people are upfront with the American public about how serious this threat is, and if it turns out that we overreacted and it isn’t as bad as it looks like it might be, then we should all celebrate. But, you know, there’s a window of opportunity to get people to start to change behaviors that could have an impact on the trajectory of this outbreak in the United States. The goal really is to try to keep the healthcare system from being overwhelmed by a whole bunch of people who can’t breathe, struggling into hospitals all at once.
So, people need to know that this is, this is a serious threat. I mean, I’m still getting pinged on Twitter by people who say, you know, this is nothing but the flu. Stop lying. Stop trying to frighten people. This is not the flu. People need to know that. And I’m glad Dr. Fauci laid it out clearly.
Ron Klain: I’m sure you’re also getting pinged by people who say, Hey, why isn’t this like, you know, chicken pox in the 1970s where we should just actually hope everyone gets it quickly and it gets over. Um, talk a little about why flattening the curve is so important.
Helen Branswell: You know, everyday hospitals in this country are running almost at capacity. Over the course of, you know, some months, somewhere between 20, 40, even 60% of Americans might be infected with this. The vast majority of them will be fine. But you know, the estimates at this time are that about 20% of people who catch this virus have severe symptoms, probably needing oxygen at the least, and, uh, about 5% need to go into critical care, which is a hugely demanding. There just literally aren’t enough critical care beds in the country. Doctors are going to be faced with the horrible choices of deciding whose lives to save effectively. If you have two people who need ventilators and you have one ventilator, you have to actually choose.
Nobody wants to be put in that position. And so, the goal is to try to keep as many people from being infected for as long as possible to try to effectively stretch this thing out so that the hospitals are dealing with fewer cases. The surge is not as great. How big the surge is, really, will tell the difference between whether this is a very bad event or a catastrophic event.
Celine Gounder: Some of the modeling would indicate we’re about 10 days behind the Italians in terms of our own epidemic here in the U.S. Are we going to be in the same boat in two weeks, and is there anything we can do to prevent that?
Helen Branswell: We don’t have a good sense of how much of this virus is spreading in the United States at the moment because of the terrible fiasco over the testing. I don’t think the amount of testing that’s going on now is sufficient to give people a good handle on where the emerging hotspots are. I mean, we all know about Seattle. We know about, uh, New Rochelle, New York, and Florida, but there are undoubtedly other places that are going to start lighting up soon.
And without knowing where they are, it’s really kind of hard to get a sense of where the country is in the trajectory of this thing. But it is very clear it’s coming. It’s coming soon. And the time to act is now.
Ron Klain: So, this week President Trump spoke about travel restrictions. Have a listen to what he said:
To keep new cases from entering our shores, we will be suspending all travel from Europe to the United States for the next 30 days.
Ron Klain: So, Helen, do you think there is a role for travel restrictions at this stage?
Helen Branswell: They buy you a little time, but not a lot. Travel restrictions now I think might have even less benefit, when you think about it. They seem to be premised on the notion that it’s not here and we need to keep it from getting here, but of course it is here. And so those kinds of travel restrictions may slow additional importations, but that doesn’t mean the virus isn’t already spreading in the United States.
So, since I’m on here with you, Ron, I had a question for you, if you don’t mind. I’m wondering how clearly you think the power brokers in Washington see this situation. You know, when I look down the line, I see the possibility that retail is going to shutter effectively because people are going to hunker down, and they’re going to be a lot of people who are temporarily unemployed for a while coming up. And typically, these are folks who don’t have the income to put away months worth of food. Are the policymakers aware of that? Are they making plans to effectively, you know, ensure the survival of these people?
Ron Klain: This week has been a real turning point on Capitol Hill. Congress got a confidential briefing from the doctor that treats members of Congress, and he told them in that confidential briefing, the between 70 and 150 million Americans could get coronavirus. So, I think that we are going to see a move very soon through the Congress, some kind of economic relief package aimed at individuals who lose wages, aimed at businesses who lose business, perhaps tax cuts- that’s what president Trump has proposed. But absolutely right, Helen. This is the next frontier in the policy action, and I think we’re going to see this really start, uh, when Congress comes back from going home for a few days.
Helen Branswell: Obviously, you know, people are going to die in this outbreak, but there are going to be consequences that are more widespread than that. You know, the downstream impact of having so many people sick and so many measures taken. I mean, people really need to be thinking about the other damage this does.
Ron Klain: You know, it’s interesting because in some ways the goal of economic policymakers and public health policymakers might be at odds with one another. From the perspective of economists, the sooner the coronavirus moves through our country, the better. The more it would be like a temporary disruption, the better for business or whatnot. But as we’ve been talking about in this episode, the goal of public health experts is to flatten the curve, is to actually make this a smaller problem, but a longer problem, to push the cases out. And that’s going to obviously be better for our health care system, be better for our public health, but that’s going to make the economic impact longer lasting and more substantial.
Celine Gounder: Helen, have you been speaking to healthcare workers here in the United States and, and you know, are they worried about what’s coming and what are they saying to you?
Helen Branswell: I think one of the things people are really concerned about is the supply of PPE in this country- personal protective equipment. That means health workers are looking at the scenario, down the road, hopefully, but not far enough down the road, where they have to make decisions about how to do things without infecting themselves. That’s a terrible circumstance to find oneself in, and I hope we don’t get there, but I do think that there’s a possibility that it’s coming.
Ron Klain: So, Helen, thank you very much for joining us. It’s great to have you on the podcast. We really appreciate your time.
Helen Branswell: Thanks for having me.
Ron Klain: We’re thrilled to be joined on the “Epidemic” podcast by one of my personal heroes, Dr. Craig Spencer, who is at the Columbia University Medical Center. He coordinated the Doctors Without Borders national epidemiological response in Guinea during the Ebola outbreak. And if you own a television set or a radio, or listen to any kind of media, you know that during that outbreak, Craig not only went to Africa to fight the disease, he himself became a patient and was treated back here in the United States successfully five years ago. Amazingly since then, he’s continued his generous and heroic work providing medical care in the Caribbean, Central America, and most recently for Doctors Without Borders in Burundi, East Africa. He served on a medical search and rescue boat in the Mediterranean, helping refugees there. In 2019, he was elected to the Board of Directors of Doctors Without Borders for the United States. So welcome to the podcast, Craig.
Craig Spencer: Thank you, Ron. Thank you, Celine.
Celine Gounder: Craig, it’s really an honor to have you on the show. I’m sort of curious where in Guinea were you based? Because I actually spent two months out there, but I didn’t head over until you’d already come back, so we must have just missed each other.
Craig Spencer: Yeah. I think that’s a pretty common theme amongst many of us that were there. Um, I was initially in Gueckedou in the, uh, bullet treatment centers. Um, so most of my time was spent either at home, um, or at, you know, our little, uh, MSF compound, or walking along the streets down to the Ebola treatment center, right in town. And I spent the majority of my day, probably 12 to 14 hours inside the treatment center providing care.
That was the first time I was there in September/October 2014. I went back in March knowing that after having been infected, um, people were going to assume that I was an expert on a disease that quite frankly, I only saw within the walls of an Ebola treatment center. So, I went back in a capacity as an epidemiologist in 2015, with antibodies in tow. One, to really continue the fight against the response, but also so that I understood more of what was happening outside the walls of the Ebola treatment center, and that was really important for me to understand the transmission and learn a lot more about diseases, like the spread.
Celine Gounder: What went through your mind the first time you arrived there? Was it what you expected?
Craig Spencer: You know, quite honestly, the first couple of days that I was working within the bullet treatment center, it was a mix of curiosity and empathy to really help out people that weren’t getting the care that we, that we all know, they, uh, they need it. But the international response was quite slow at that time.
And quite frankly, it was just a lot of fear. One story that I tell a lot is that in the United States, I work in an emergency room. It’s busy. My mom always told me, take care of your nurses. That’s how you’re going to be a good doctor. So at least once a shift, I try to put in my own IV. I’m really good at putting in intravenous lines. And for the first few days that I was in Guinea, I tried multiple times and I missed, and I tried to convince myself that it was because of the gloves. And I tried to say that it was for something else, but what it really was, it was for the fear.
Ron Klain: So Craig, I want to talk about this a little bit from the kind of the layperson’s perspective as they start to think about this. We think about doctors and nurses as the people who take care of all of us patients, but in an epidemic, you doctors, nurses, other healthcare workers are the people who are really most at risk of becoming patients themselves. So, what do you think about when you are sent to help respond to an epidemic, whether that’s overseas or potentially now this challenge of coronavirus here in the U.S.?
Craig Spencer: You know, I think that the majority of my colleagues and the people that I work with, whether it’s domestically or internationally, we all recognize, especially for, for my group that’s in the emergency department or working as part of international NGOs that are providing healthcare and other places, we know that there’s a risk, but we all recognize that in the process of doing that really important part of our job, which is providing care to people who need it most wherever they need it. And I think that when you ask people like myself and many of my colleagues, we feel we have a moral obligation to provide this care, whether it’s here in the U.S. or whether it’s somewhere internationally.
The story I have to give is that people ask me why I would go to West Africa to provide care to people who are dying from a disease, you know, that had 60 to 80% mortality. Well, if we’re not doing it, then who is? Especially at a time, when you think about the number of doctors that were in Guinea, Liberia, and Sierra Leone, the three countries hit hardest by the Ebola crisis in 2014-2016, the number of doctors in those three countries combined was less than the number of doctors in the one hospital where I was treated in New York city.
I think that there’s this understanding that we have this duty to provide care to whomever it is, wherever they are in the world. Now, I think that’s reliant on a couple of other things. One, there’s a lot of uncertainty around, you know, who are the patients? What are the symptoms, is it spread differently than things like Ebola or HIV?
And that’s causing a little bit of uncertainty for people on the front lines. I think the other thing, too, is you want to make sure that you have the right access to personal protective equipment. You have the right training. We know that there’s always a risk, but if we have those things in place, then I think people like my healthcare colleagues are a lot more comfortable providing the care that we think all people deserve, regardless of where they are in the world.
Celine Gounder: So, let me ask you this. What is a health care worker’s obligation to care for someone in an epidemic, especially one involving a new or untreatable infectious disease? You know, I’m thinking a little bit about, um, HIV as well. And in the early days there was a lot of concern about, you know, was it safe for healthcare workers to be caring for these patients?
Craig Spencer: Myself personally, I think that we do, as healthcare providers have a moral obligation to provide care if we are provided with the preparation and really the understanding of how we can do that in the safest way for ourselves, as well as for the people we’re taking care of. So when I think back on kind of our moral obligation to respond here in the U.S., I think about the people I worked with in Guinea, and really the extents that they went to take care of people, even if their preparedness wasn’t to the same level of what we have here in New York City or throughout the country.
I try to think about the national staff that worked in situations like Ebola and how they really stood up at a time when we needed them to provide care to people in their communities. And so, I think that’s one thing. Another caveat, when we think about this moral obligation, is what are going to be the downstream impacts, not only on that provider, but on their family, on their institution.
When we think about, especially with coronavirus, there’s certainly a risk of fear leading to human error, which could potentially increase transmission. But the other thing is that we don’t know enough in terms of how to, kind of, prepare people after they’ve taken care of a patient or possibly been exposed.
I think this can have downstream effects on people who may be living with or interacting with family members who have immunocompromised, so people on medications for transplants or other vulnerable populations. I think that there’s a couple of other considerations that need to go into this that we need to think about before we, I guess, force people to provide care.
Ron Klain: I think that’s a great frame for it. I mean, it’s, it’s one thing for really brave and generous people like you and Celine to make an intentional choice to go to Guinea, to help people with Ebola and knowing what you’re getting into. But right now, healthcare workers all over our country have to deal with those patients with coronavirus. How do you think about that challenge and frankly, how well-prepared they are to deal with that right now?
Craig Spencer: I think for me the concern is more, what is going to be the impact on our larger healthcare system if providers are exposed, or providers are positive, or providers don’t feel comfortable providing care for whatever reason. What is going to be the larger impact on our ability to provide care, and what does that mean for the heart attacks, and the breech deliveries, and the patients that come to us every single day with other presentations that aren’t coronavirus, right?
We think that the mortality from non-Ebola in West Africa was likely higher than the mortality from Ebola because of a bulldoze impact on the healthcare system. How are we thinking about that here, and how are we preparing for that potential inevitability of coronavirus cases impacting the normal day to day activities in our emergency rooms or ambulatory care clinics, our urgent cares, or in our catheterization labs?
Ron Klain: Craig, let’s just stick with this for a second. Cause I think this is a huge question right now in Washington state, where you have a number of cases, people being treated in hospitals, and the question of whether or not the people who are treating them need to themselves be quarantined.
If they do, can they provide care to other patients? If they can’t provide care to other patients, who’s going to step in and replace them in providing care? How do you deal with these people coming to and from the hospital? One thing that’s interesting about this is around the world right now, the countries that have seen the largest cluster of cases are countries with pretty advanced healthcare systems- China, South Korea, Italy, Japan. But the risk here is also the coronavirus spreads to countries with less developed healthcare systems, and particularly I think a lot of experts are worried about the risk of coronavirus in Africa and spreading across the continent of Africa. With your Doctors Without Borders hat on, how do you think about that and how should the international community prepare to respond to the possibility of a coronavirus epidemic in someplace like Africa?
Craig Spencer: I was working recently with one of my colleagues who’s from the Congo, and she said, looking at that map, you’d think that Sub-Saharan Africa is immune to the coronavirus, and that’s not because there aren’t cases there, right. It’s because there’s not a lot of testing capacity to prove that there are cases. My concern is that the, the overwhelming focus on the domestic will lead us to really not focus enough or overlook the importance of spread in places like Sub-Saharan Africa, or in places in Latin America and other places where the infrastructure and the resources just don’t exist at the same level, so we suspect that the mortality would likely be higher in those places. Externally, there is a huge risk and we also have an obligation to think about how we help people around the world in places that don’t have the same access to resources and staffing and, um, you know, the high level of, uh, of quality care that we’re able to provide here in the U.S.
Celine Gounder: With respect to the Ebola response in Guinea, what was done especially well that you think we can learn from?
Craig Spencer: I do think that once we did mobilize, we did do a really good job of starting in clinical trials in the middle of an outbreak of one, you know, this really scary viral hemorrhagic fever. And as such, now we have a vaccine that is extremely effective. We have therapeutics where none existed when I was taking care of patients in 2014 and 2015, so that with the more recent outbreak in Congo, we were able to use a vaccine. We were able to use these novel therapeutics that quite frankly, I didn’t have, that could have saved so many lives in West Africa in 2014 and 2015. Our ability to get together and find a way to do research and you know, look at these ethical issues of, of doing research within an outbreak. This was really unprecedented and it’s one of the things that we did extremely well.
Ron Klain: Well Craig, thank you so very much for joining us. As always, it’s a great honor and privilege to chat with you and we appreciate you informing our audience about your experience, and about your insights about this coronavirus that we’re facing now.
Celine Gounder: Thanks, Craig.
Craig Spencer: Thank you, Ron. Thank you, Celine
Ron Klain: Every week on the “Epidemic” podcast, we’d like to answer a couple of questions from listeners. Record an audio file on your phone with your question and then email it to Celine and I at hello@justhumanproductions.org. That’s hello@justhumanproductions.org. Our first question today is from Kay.
Hi, this is Kay in Madison, Wisconsin. My 89-year-old mother lives 250 miles from me in a 15-story high rise with two elevators. She lives independently but eats breakfast in the communal dining room. As a group, she and her neighbors are vulnerable to the worst effect of this virus. Right now, there’s only one confirmed infection in her large city, but that’s bound to increase.
We thought maybe she should come to my house when that happens. I could provide all her meals and assistance, but I am hearing that what epidemiologists call non-pharmaceutical interventions matter most before the infection numbers are rising quickly. So, should we take this step now that would isolate her from shared spaces before her neighbors get sick?
But she would be living with two other adults. My husband works on a large campus and travels some. We will increase our social distances, but inevitably she’d have more secondhand contacts than if she isolated herself in her tiny apartment. Assuming she’s willing to consider either option, how do we decide what is safest for her? We would love some guidance. Thanks. Love your informative show.
Celine Gounder: So, Kay, you know, it’s a really challenging situation because the elderly are definitely the highest risk group. Your mom at 89 is, is certainly high risk for severe disease and even death from the coronavirus. And so certainly you would want to be minimizing her contact with others.
I think the best thing to be doing is that people probably need to be sticking to their own units within the facility. And obviously the usual stuff, which is using lots of hand sanitizer, soap and water to keep clean. My own father in law lives at a memory care facility south of Tucson in Arizona, and I had a conversation the other day with the director of the facility, and they’re really not sure what to do, so they are quite concerned and are doing what they can in terms of screening visitors.
Here’s a question. Mayabot Gregerson emailed us.
Why don’t state health departments take public health guidance on COVID-19 from WHO or academia, rather than the CDC and federal government? The feds are dispensing vague and ineffective guidance. What legal or other consequences would there be for state governments if they were to follow the recommendations of their own experts rather than the CDC and White House?
Ron, what do you think? Would there be repercussions?
Ron Klain: The CDC has not really stepped up to provide that kind of guidance, and as a result, state and local governments are going their own way. You’ve seen that first on the testing issue where, for example, in the state of New York, governor Andrew Cuomo ordered state labs to proceed with testing even before CDC had signed off on that.
You’re seeing that with announcements from a variety of state and local authorities shutting down large local events, shutting down sporting events. So, I don’t think state and local governments are awaiting guidance from CDC. And I do think this is a case where CDC hasn’t really stepped up and provided clear enough, fast enough, precise enough guidance.
There’s no real consequences for that- the CDC guidance is always advisory. I think it would be better if CDC were issuing that kind of guidance. I think the state and local public health officials are looking for it, but they’re not getting it, so they are taking the lead in fighting this epidemic. Our last question, it was sent by email from Josh Dolezal. Josh wrote us and said,
I teach at a private liberal arts college in Iowa, and every day more campuses are closing or moving to online classes. Is there any evidence that those measures really slow the spread of covid? In your minds, are these extreme measures justified?
Celine Gounder: So, there’s been a lot of debate about school closures in general, um, and whether young people are major drivers of the infection. And part of the problem is we just don’t know. It’s not an unreasonable measure if you’re trying to reduce community spread, and it’s not to protect the students attending college so much. It’s really to protect the elderly and people with chronic medical conditions who are around college campuses, and that actually includes a lot of the people who teach and work there.
The cons of closing down a public school, a grade school, a high school are very different from closing down a liberal arts college or university for a period of time. You know, if you’re talking about public schools, a lot of kids depend on free or reduced cost lunches and its childcare. So, that’s not the same situation as you’re talking about with young adults, you know, 18 to 22 who are attending colleges and universities.
Ron Klain: You know, Celine, one thing that does concern me, though, about some of these college closures is that many students get their healthcare services through their college, uh, either through paying a fee to get those services or through buying an insurance plan that’s kind of tied to the college. And I think one question we’re going to face is, if the colleges closed and send the students away, do they have some access to healthcare where they’re being sent to? Uh, and will their healthcare coverage help pay their medical bills where they’re being sent to? So, even closing these universities is complicated and has benefits, but also will have some negative effects.
Celine Gounder: And finally, I know a lot of you are also wondering about the new travel ban with Europe. There’s still some confusion about what they actually mean, but here’s what I can tell you. These restrictions apply only to people who are not American citizens. And even then, you’re exempt if you have close family who are American citizens or permanent residents.
You’re exempt if you’re in the U.S. military or the spouse or child of someone in the military. The travel ban doesn’t cover all European nations, only the 26 that allow free movement across borders. So this doesn’t include travel to countries like the UK and Ukraine, among others. So there are lots of loopholes, as was the case with the restrictions on travel to China. You’re treated differently depending on the color of your passport, but the virus doesn’t check passports.
Celine Gounder: We really haven’t seen many coronavirus cases imported from Europe into the United States, so it’s not clear that these travel restrictions will do anything to prevent the spread of coronavirus. It’s already here.
“Epidemic” is brought to you by Just Human Productions. Today’s episode was produced by Zach Dyer and me. Our music is by the Blue Dot Sessions. If you enjoy the show, please tell a friend about it today, and if you haven’t already done so, leave us a review on Apple podcast. It helps more people find out about the show.
You can learn more about this podcast, how to engage with us on social media, and how to support the podcast at epidemic.fm. That’s epidemic.fm. Just Human Productions is a 501(c)(3) nonprofit organization, so donations to support our podcasts are tax-deductible. Also, check out our sister podcast, “American Diagnosis.” You can find it wherever you listen to podcasts or at americandiagnosis.fm where we cover some of the biggest public health challenges affecting the nation today. In season one, we covered youth and mental health, in season two, the opioid overdose crisis. And in season three, gun violence in America.
Celine Gounder: I’m Dr. Celine Gounder.
Ron Klain: And I’m Ron Klain.
Celine Gounder: Thanks for listening to “Epidemic.”